Monsoon diseases and how to stay safe
Table of Contents
Across India—from the Himalayas in the north to the Indian Ocean in the south—the monsoon arrives in many shades: gentle in some places, torrential in others. With the rains come new water bodies, overflowing drains, and humid air—and with them, a predictable rise in certain infections. Here’s the reality check: India shoulders a major share of the world’s mosquito-borne burden, contributing roughly a third of global dengue and a notable slice of global malaria, and those risks intensify during the rainy season. Your exposure to multiple infections can be up to twice as high in monsoon compared with other seasons, mainly due to humidity and environmental contamination.
Surprising fact: The risk of being exposed to multiple infections is about two times higher during the rainy season because warm, wet conditions help pathogens thrive.
1. Introduction of
rainy season diseases
India’s vast geography means the monsoon “hits differently” across regions—early surges in the Konkan, late bursts in the Gangetic plains, and intermittent showers in the Deccan. Wherever you are, one pattern is consistent: more standing water and more humidity translate into higher disease risk. Mosquitoes breed in newly formed clean and dirty water pockets; drains overflow; drinking water lines may get contaminated. That’s why each monsoon demands the same trio: awareness, prevention, and early care.
Why this matters:
Humidity and waterlogging: More breeding sites for mosquitoes and easier spread of microbes.
Sanitation stress: Floods and leaks can mix sewage with potable water.
Behavioral shifts: People spend more time in crowded, poorly ventilated spaces, aiding respiratory spread.Key seasonal takeaway:
Mosquito-borne illnesses rise: Dengue, malaria, chikungunya.
Waterborne illnesses spike: Typhoid, cholera, diarrheal diseases, hepatitis A/E.
Skin and respiratory issues increase: Fungal infections, colds, influenza-like illness.
Many Indian cities report sharp monsoon spikes in dengue, malaria, and chikungunya when intermittent rains cause water to stagnate, creating ideal mosquito breeding conditions.
2. Why rainy season increases disease risk
Humidity and warmth:
Effect: Favors growth of bacteria, viruses, and fungi; increases transmission chances.
Impact: More colds/flu, mold-triggered allergies, and fungal skin infections.Stagnant water and vector breeding:
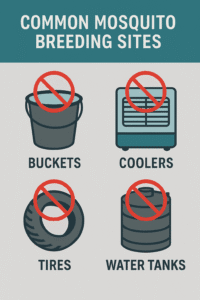
Effect: Water in pots, tires, coolers, rooftops, and puddles encourages Aedes (dengue/chikungunya) and Anopheles (malaria) mosquitoes.
Impact: Predictable surge in vector-borne diseases during monsoon months.Floods and sanitation failures:
Effect: Overflowing drains and mixed sewage contaminate drinking water.
Impact: Increased typhoid, cholera, diarrheal disease outbreaks.Compromised food and water safety:
Effect: Street food, uncovered produce, and ice made from unsafe water elevate risk.
Impact: Gastrointestinal infections, hepatitis A/E.
Bottom line: Warm, wet conditions + waterlogging + sanitation stress = higher risk across waterborne, vector-borne, and respiratory illnesses.
3. Common rainy season diseases
3.1. Waterborne diseases
Cholera
Cause and spread:
Vibrio cholerae via contaminated food or water, often after flooding or sewage leaks.
Symptoms: Profuse watery diarrhea, vomiting, rapid dehydration.
Prevention: Safe water (boiled/filtered), hygienic food handling, handwashing, prompt oral rehydration at first signs.Immediate actions:
Start ORS early: Prevent dehydration while seeking care.
Seek medical help: Severe dehydration can be life-threatening.
Typhoid
Cause and spread:
Salmonella Typhi via contaminated water/food and poor sanitation.
Symptoms: Prolonged fever, headache, abdominal pain, weakness; constipation or diarrhea.
Prevention: Boiled/filtered water, cooked fresh food, hand hygiene; typhoid vaccines exist and may be recommended in some settings.Watch-outs:
Delayed care risks: Intestinal complications if untreated.
Food safety: Avoid cut/raw street foods during heavy rains.
Diarrhea and dysentery
- Cause and spread:
Bacterial, viral, or parasitic infections from unsafe water/food.
Symptoms: Loose stools, cramps, fever; dysentery may include blood/mucus.
Prevention: Safe water, fresh cooking, handwashing, kitchen surface hygiene; early ORS for dehydration.
Children and older adults are especially vulnerable to waterborne diseases during the monsoon; strict water and food safety can significantly reduce risk.
3.2. Vector-borne diseases
Dengu
- Mosquito type and behavior:
Aedes aegypti (day-biting), breeds in clean, stagnant water found in and around homes—coolers, planters, buckets, tires. - Symptoms:
High fever, severe headache, pain behind the eyes, intense muscle/joint pain, rash, nausea; warning signs include abdominal pain, persistent vomiting, bleeding, or extreme fatigue. - Prevention:
Eliminate breeding sites weekly: Empty/scrub water containers, clear gutters and trays.
Personal protection: Repellents with DEET/picaridin, long sleeves, window/door screens.
Community action: Clean-up drives, timely reporting to municipal bodies.
Malaria
Cause and spread:
Plasmodium parasites via female Anopheles (night-biting), thriving near stagnant/dirty water.
Symptoms: Cyclical fevers with chills/sweats, headache, vomiting; can progress to severe disease without prompt treatment.
Prevention: Insecticide-treated bed nets, indoor residual spraying, repellents, drainage of stagnant water.Seasonal pattern:
Monsoon conditions—waterlogging, poor sanitation—are linked with surges; any high fever in rainy season warrants testing.
Chikungunya
- Mosquito type and behavior:
Transmitted by Aedes (day-biting), often rises in tandem with dengue.
Symptoms: Sudden high fever, severe joint pain/stiffness, fatigue; joint pain may linger.
Prevention: Same as dengue—destroy breeding sites, repellents, protective clothing.
Intermittent rains followed by dry spells can worsen outbreaks by allowing stagnant water to persist—sustaining both Aedes and Anopheles populations.
3.3. Airborne and seasonal flu
Common cold and viral fevers:
Why it rises: Humidity and crowding support respiratory virus spread; mold and dampness aggravate allergies and asthma.
Symptoms: Sore throat, cough, fever, body aches, runny nose.
Prevention: Hand hygiene, avoid close contact when ill, good ventilation, mask use in crowded indoor settings if needed.Influenza in humid weather:
Seasonal flu can circulate efficiently in monsoon conditions; vaccination where recommended reduces risk for vulnerable groups.
3.4. Skin and fungal infections
Common issues:
Athlete’s foot and ringworm: Itchy, scaly rashes in moist areas (toes, groin, underarms).
Folliculitis/boils: Infected hair follicles due to sweat and friction.
Triggers: Damp clothing, prolonged wet shoes/socks, poor ventilation, shared personal items.Prevention tips:
Keep skin dry: Pat-dry folds after bathing or getting drenched; change out of wet clothes quickly.
Breathable clothing: Prefer loose cotton; avoid tight synthetics.
Foot care: Open-toed or breathable footwear; antifungal powder if prone; avoid walking barefoot in puddles.
Do not share: Towels, combs, socks, or footwear to prevent spread.
High humidity traps sweat and moisture on the skin, creating ideal conditions for fungal overgrowth—timely drying and breathable fabrics make a big difference.
4. Early signs and when to seek medical help
Dengue warning signs (urgent):
Look for: Severe abdominal pain, persistent vomiting, bleeding gums/nose, extreme fatigue, restlessness; seek immediate care.Malaria red flags:
Look for: High-grade fever with shivering/chills, headache, vomiting, jaundice, confusion, breathing difficulty—test and treat early.Severe dehydration:
Look for: Intense thirst, very little urine, dark urine, sunken eyes, dizziness; start ORS and seek care promptly.Gastrointestinal alarms:
Look for: Profuse watery diarrhea, blood in stools, severe abdominal cramps, high fever—urgent evaluation.Respiratory concerns:
Look for: Shortness of breath, chest pain, persistent high fever—seek medical attention.
Do not self-medicate with antibiotics for undiagnosed fevers or diarrhea. Accurate testing guides the right treatment and helps prevent antimicrobial resistance.
5. Prevention strategies
Personal hygiene:
Handwashing: Use soap before eating/preparing food and after using the toilet.
Rain routine: Shower and change into dry clothes after getting drenched.
Surface hygiene: Disinfect kitchen counters and high-touch surfaces regularly.Food and water safety:
Water: Drink boiled/filtered water; store in covered, clean containers.
Food: Eat freshly cooked meals; avoid raw salads, cut fruits, and uncovered street food during heavy rains.
Produce prep: Wash fruits/vegetables thoroughly; peel when possible.Mosquito control:
Home: Remove stagnant water weekly; scrub containers to dislodge eggs; keep tanks covered.
Personal: Use DEET/picaridin repellents; wear long sleeves and light-colored clothing; install window/door screens.
Night protection: Sleep under insecticide-treated nets in malarial areas.Vaccinations (where recommended):
Typhoid: Consider vaccination based on local guidance.
Hepatitis A: Vaccine available in many settings; ask your clinician.
Influenza: Seasonal vaccination reduces risk for high-risk groups.
Even small amounts of clean standing water (planter trays, AC drip trays, cooler pans) can breed Aedes mosquitoes—check and clear these spots every week.
6. Home remedies and first aid with caution
ORS for dehydration:
Best choice: Use WHO-standard ORS sachets with safe water.
If packets are unavailable: A commonly advised home mix is 1 liter of clean water with 6 level teaspoons of sugar and 1/2 level teaspoon of salt—measure carefully and use clean water. Start small, frequent sips, and seek medical advice if symptoms persist or worsen.Hydration pointers:
Go slow: Frequent small sips reduce vomiting.
Replace losses: Continue ORS while diarrhea lasts; watch for urination and thirst to improve.
Children and elders: Prioritize early ORS and medical guidance.Herbal supports (adjuncts, not cures):
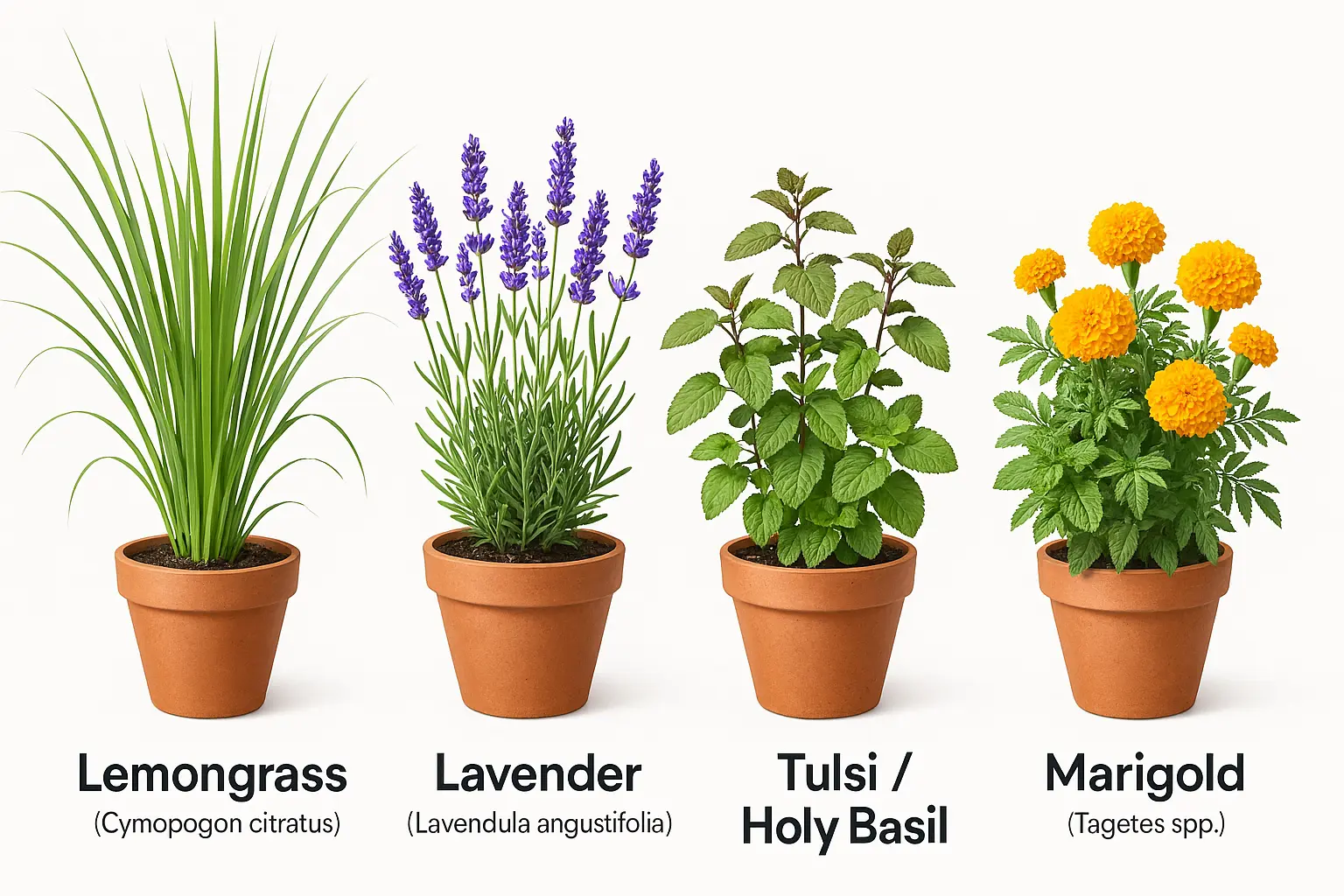
Ginger and tulsi: Warm infusions can soothe sore throats and nausea.
Turmeric: Anti-inflammatory when used in food; do not use as a substitute for medical treatment.
Safety first: If fever is high or persistent, or there’s vomiting/dehydration, consult a doctor promptly.Skin care first aid:
Dry and protect: Keep affected areas dry; use antifungal powder on prone zones.
Avoid steroids: Do not self-use steroid creams for rashes; they can worsen fungal infections.
Medical help: See a dermatologist if rashes persist beyond a few days or show pus, spreading redness, or severe itching.
Many “ORS-like” drinks are not medical ORS. When in doubt, choose WHO-ORS sachets and clean water, and consult a clinician if dehydration is severe or persistent.
7. Public health measures and community action
What authorities do in monsoon:
Vector control: Fogging in hotspots, larvicide in drains, indoor residual spraying in malarial zones.
Water safety: Chlorination, water quality monitoring, outbreak surveillance.
Public messaging: Alerts on fever testing, dengue prevention, and hydration.What communities can do:
Weekly clean-ups: Jointly remove stagnant water from shared spaces, rooftops, and lanes.
Report hazards: Flag clogged drains, overflowing garbage, broken waterlines to municipal teams.
Neighborhood watch: Track fever clusters; support testing and prompt care.
Cities consistently record spikes in dengue, chikungunya, and malaria during monsoon, and local bodies urge public participation to eliminate breeding sites and seek early testing for fevers.
8. Myths versus facts about monsoon diseases
Myth: Dengue spreads directly from person to person.
Fact: Dengue spreads via Aedes mosquitoes; it doesn’t pass by touch or sharing food. Control breeding sites and prevent bites.Myth: Clean homes don’t have mosquitoes.
Fact: A tiny amount of clean water in planters/coolers is enough for Aedes to breed. Weekly checks are essential.Myth: Only dirty water breeds mosquitoes.
Fact: Aedes prefer clean stagnant water; Anopheles may breed in varied water types. Eliminate all stagnant water.Myth: Antibiotics cure all monsoon fevers.
Fact: Many monsoon fevers are viral (e.g., dengue, influenza). Unnecessary antibiotics can harm and fuel resistance.Myth: If diarrhea stops, hydration isn’t needed.
Fact: Rehydration should continue until thirst, urination, and energy return to normal.
9. Conclusion
Monsoon brings relief and renewal—but also predictable health risks that we can prevent. Keep water and food safe, eliminate mosquito breeding sites, stay dry and ventilated, and seek testing early for any fever, diarrhea, or concerning symptoms. Share these practices at home, in your building, and across your neighborhood—awareness and small routines save lives.
- Quick safety recap:
Eliminate water weekly: Planters, coolers, buckets, AC trays, tires.
Drink safe water: Boiled/filtered; skip raw salads and cut fruits outside.
Protect from bites: Repellents, full sleeves, screens, and bed nets.
Act early: High fever, vomiting, bleeding, or dehydration demands prompt care.
If this guide helped you, share it with friends and family—community awareness is the strongest antidote to monsoon outbreaks.
10. Citation
- World Health Organization (WHO) – https://www.who.int
- National Vector Borne Disease Control Programme (NVBDCP), India – https://ncvbdc.mohfw.gov.in/
- Ministry of Health and Family Welfare, India – https://www.mohfw.gov.in
- Centers for Disease Control and Prevention (CDC) – https://www.cdc.gov
- PubMed – https://pubmed.ncbi.nlm.nih.gov
Additional referenced material in this article includes reputable public health explainers and news-health briefings that synthesize national advisories and seasonal patterns: Medanta, Times of India, Hindustan Times, NDTV reports, and municipal updates via Free Press Journal.
FAQs
1 What are the main reasons mosquitoes enter the house?
Mosquitoes often enter homes due to stagnant water, unhygienic surroundings, open windows, and doors without screens. Water collecting in buckets, flower pots, and on rooftops provides ideal breeding spots for them.
2 Do mosquito-repelling plants really work?
Yes — plants like Tulsi (Holy Basil), Lemongrass, and Mint act as natural mosquito repellents. Their strong aroma contains compounds such as citronellal, eugenol, and menthol, which help keep mosquitoes away while adding freshness to your home environment.
3. Why does the mosquito menace increase during the monsoon?
During the rainy season, water tends to collect in pits, flowerpots, and coolers. The warm and humid weather creates ideal conditions for mosquito eggs to hatch into larvae and grow rapidly.
4. What is the easiest home remedy to make your house mosquito‑free?
The simplest method is to remove stagnant water, spray neem or lemongrass oil, and install nets on windows and doors. These steps quickly reduce the number of mosquitoes in your home.
5. what is the Difference between Dengue and Malaria ?
Dengue is caused by the dengue virus and spread by Aedes aegypti mosquitoes that bite during the day and breed in clean stagnant water. Malaria is caused by Plasmodium parasites and spread by Anopheles mosquitoes that bite at night and breed in stagnant or dirty water. Dengue symptoms include high fever, severe body/joint pain, and rash, while malaria typically presents with cyclical fever, chills, and sweating. Dengue has no specific cure—treatment is supportive—whereas malaria is treated with prescribed antimalarial drugs after diagnosis.